Call the midwife!
Spring 2016 issue
When Stephanie Duffy got pregnant, she realized she would have to call a midwife — and fast.
“I knew there was a waiting list and that a midwife was hard to get, so the second I found out I was pregnant I filled out an intake form,” says Duffy, a 33-year-old registered nurse from Calgary. “I heard back right away.”
Duffy was paired with a team from Birth Partnership Midwives, which included Tiffany Harrison, one of the first eight midwives to graduate from Mount Royal University’s new four-year Bachelor of Midwifery program in May 2015.
Harrison cared for Duffy throughout her pregnancy and when she went into labour, Harrison arrived at Duffy’s house to see her through labour and delivery. The expectant mom was able to walk around in the comfort of her own home, which she credits with speeding up her labour.
After two hours of active labour, Duffy gave birth to baby Sophia at 4 a.m. Everything went beautifully.
“After, Tiffany warmed some blankets in the dryer and tucked me, my baby and my husband into bed,” Duffy says. “She tidied everything up, put away her equipment — midwives bring a lot of equipment — and even put in a load of laundry.
“It looked like nothing had happened. I was in bed, in my own home and it was so nice. I felt like I’d really been cared for.”
Sophia, now five months old, is Duffy’s second child. Her son, now two-and-a-half, was born in hospital and, although the care there was excellent, she says the difference between the two experiences is huge. “I would 100 per cent recommend the midwifery.”
Sophia’s birth was special for Harrison, too. Although she’d already “caught” many babies in her training, it was her first as a newly registered midwife.
An old practice
For generations, women had babies at home, attended by midwives. Beginning around the turn of the last century and into the 1930s, however, birthing was transitioned out of homes and into hospitals.
“Women have sought throughout the years to make it a non-medical event,” says Mary Landsiedel, a faculty member and program coordinator in the Mount Royal Midwifery program, and a registered midwife of 10 years.
For decades, midwives remained on the margins. That began changing slowly in the ‘60s, ‘70s and ‘80s with the rise of feminism and a growing interest in natural and home birth. Alberta began regulating midwifery in 1998, but women who wanted midwifery care still paid for it out of their own pockets — about $3,500, a cost many couldn’t afford.
In 2009, Alberta Health Services (AHS) began funding a fixed number of “courses” of midwifery care, in which registered midwives are paid a single fee for prenatal, labour, delivery and six weeks of postnatal care.
In September 2015, Health Minister Sarah Hoffman announced that AHS would fund up to 400 more courses of care, for a total of 2,774 midwife-supported births.
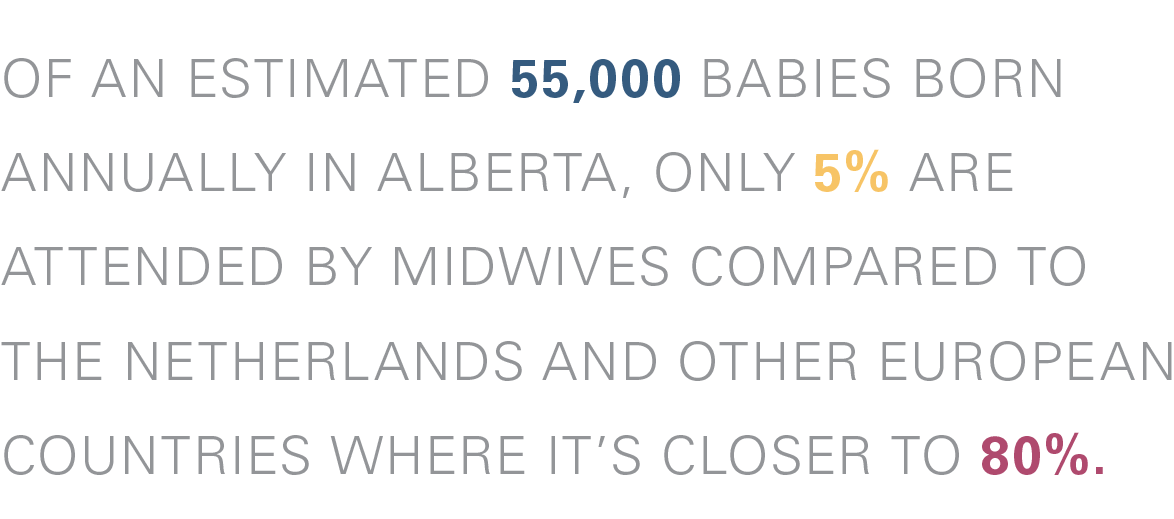
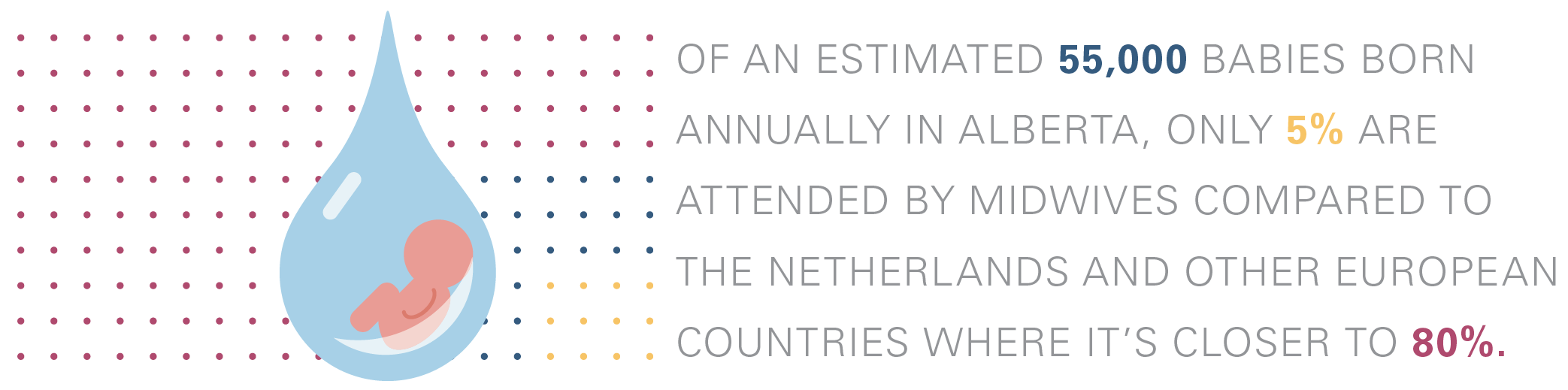
To put that in perspective, of an estimated 55,000 babies born annually in Alberta, only five per cent are attended by midwives. Compare that with the Netherlands and other European countries, where it’s closer to 80 per cent.
“The demand for midwives is huge,” says Pamela Nordstrom, director, School of Nursing and Midwifery at Mount Royal.
Currently, there are 1,900 pregnant women on the wait list for a midwife, and only 106 registered midwives in the province, says Lolly de Jonge, CEO of the Alberta Association of Midwives (AAM).
“Not all midwives are operating to capacity,” she says. “We’ve got the supply of midwives to meet some of that need, we’ve got the demand from the clients, but the funding has been capped.”
The AAM, currently in funding discussions with AHS, wants the model to change so that, “maternity care dollars follow the woman,” says de Jonge. In other words, a mom-to-be could choose to deliver a baby in a hospital with a doctor, or opt for midwifery care at home, in a hospital or in a birth centre.
Danica Sharp, director, Provincial Midwifery Services for AHS, declined to comment on lifting the cap on midwifery funding while talks are ongoing. “I want to reinforce that midwifery is an incredible and important service,” she says. “We are working hard to expand midwifery services across the province.”
Despite differences, it can be agreed that women living in rural, remote and vulnerable communities need better access to midwifery care, as most midwives are based in the Edmonton-Calgary corridor.
“It’s important to AHS to have an Alberta school graduating Albertans, and we’re hoping (new midwives) will return to their communities,” says Sharp.
The midwifery difference
Launched in September 2011, Mount Royal’s Bachelor of Midwifery program is the first and only one in the province, and the seventh of its kind in Canada.
“Just getting into the program is extraordinarily challenging,” says Nordstrom.
The requirement is a perfect 4.0 (grade point) average and over 200 people apply every year. Originally, there were to be 20 seats in the program, but because there aren’t enough registered midwives in Alberta to teach student-midwives as they go through intensive, community-based preceptorships in second, third and fourth year, only 12 (students) are accepted each year.
Like most would-be midwives entering the program, Tiffany Harrison had previous careers. Formerly an interior designer and an ophthalmology technician, she’d always been fascinated by pregnancy and birth, but publicly funded midwifery care wasn’t available when she had her own children, now 11 and 15. She says, the “exceptional care” she got in hospital inspired her to become a nurse.
But when Harrison was accepted into the Mount Royal Bachelor of Nursing program, she heard about the new Midwifery program and immediately switched.
“Being a new program, there were growing pains, but everyone — from the professors through to the dean — was there to support me,” says the 40-year-old. “And I had phenomenal preceptors.”
Now a full-time midwife, Harrison might work up to 18 hours a day or be on call ‘round the clock. Friends and family know she often has to drop everything to go deliver a baby.
“It doesn’t even feel like it’s work. Sometimes I have to pinch myself that I’m working in this field. It gives me so much joy,” she says.
Bachelor of Midwifery graduate
The best part of being a midwife, she adds, “is being of service to women, be able to support them, be present and be of service in this amazing experience.”
Continuity of care is a big part of that support, says Landsiedel. Midwives have fewer patients than doctors, their appointments are longer and they get to know their expectant mothers well.
“With the midwives, I got to know them really well during my pregnancy,” says Duffy. “When Tiffany came to our home that night, I knew her. We had a relationship. I trusted her.
“I had excellent care in the hospital when my son was born, but there were so many people involved … You’d just get to know someone and with a shift change you’d start all over again. Labour is a really intense experience and you’re doing it with strangers.”
She was especially grateful for the postpartum care. After her son was born in hospital, they went home two days later and a public health nurse visited once.
“Then you’re on your own. Tiffany came back eight hours later and helped me with breastfeeding. She came back the next day, too,” says Duffy, adding that Harrison was available to visit or answer any questions for six weeks after that.
“It was so nice to have the same person who knew my whole story, knew my husband and my son. She cared for the whole family.”
Read more Summit
Breaking Inactivity
Put down that book, give up the gaming and turn off the tube. Physical literacy is more than a buzzword — it’s a fundamental skill set that could go the way of the dinosaur if we don’t start moving (literally) in the right direction.
READ MORE